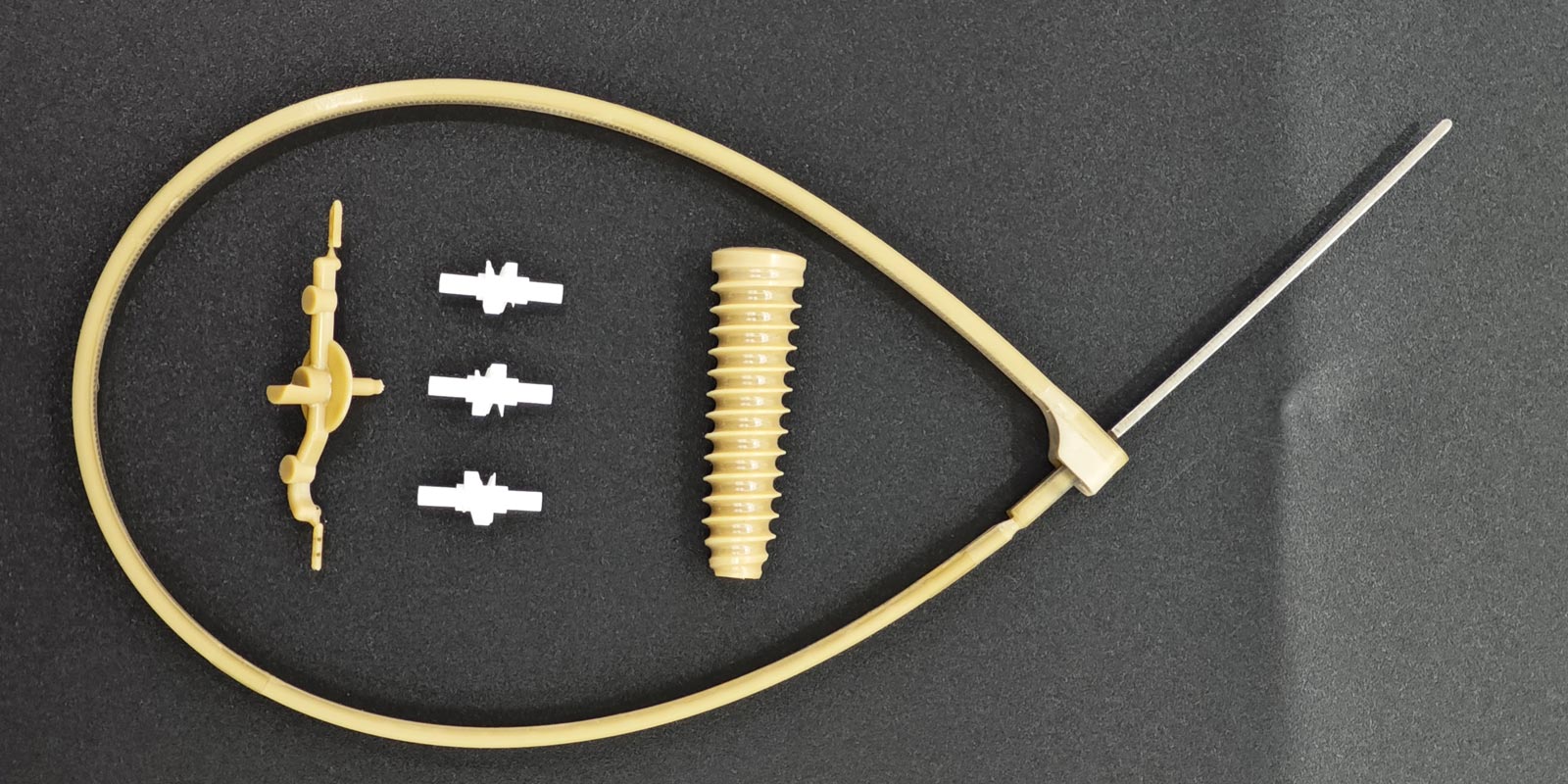
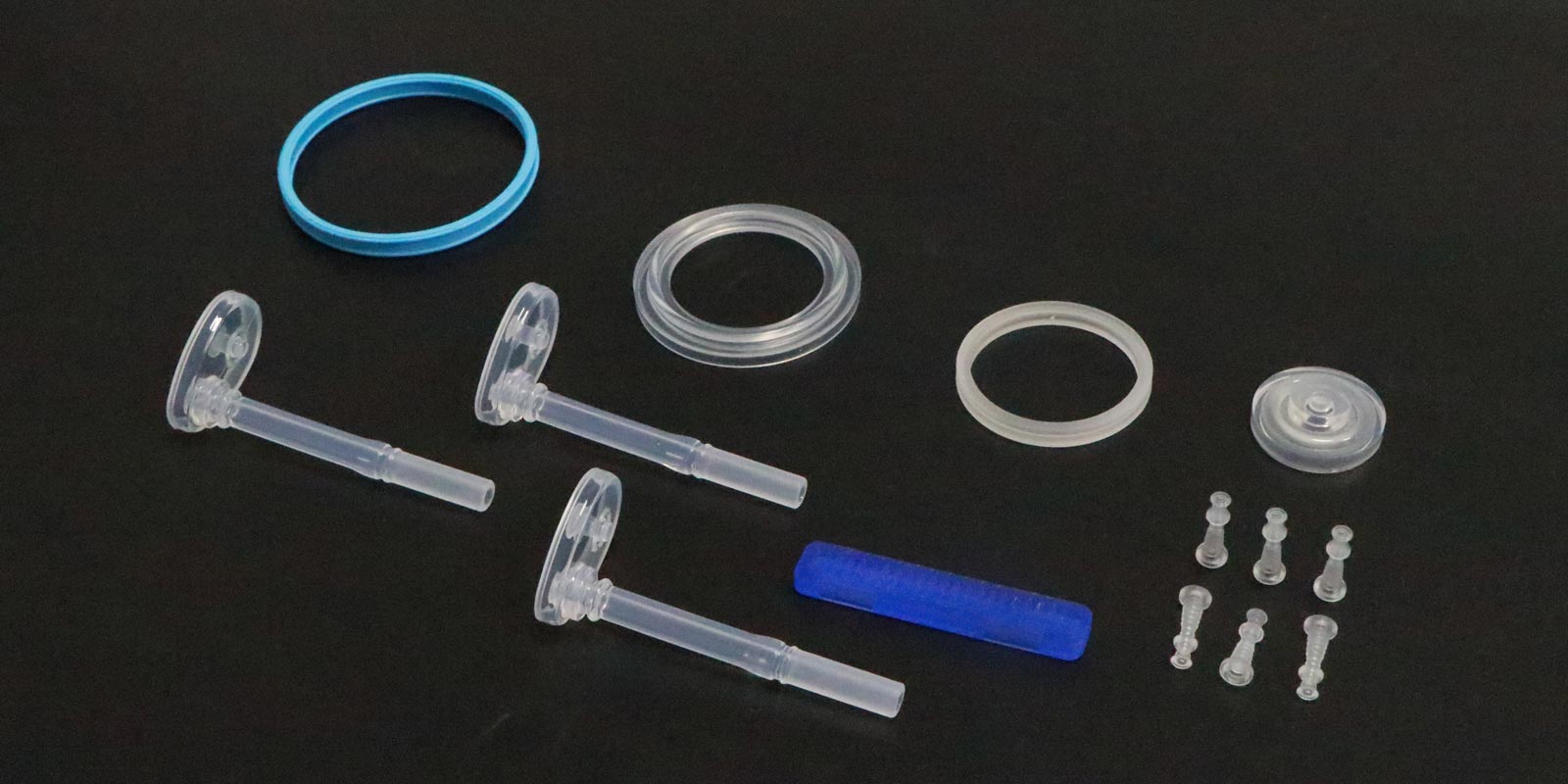
Medical injection-molded products, ranging from disposable syringes to complex surgical instruments, play a critical role in patient safety and treatment efficacy. The precision and stability of injection molding directly determine product performance. However, quality control in medical injection molding involves complex interactions across multiple stages and factors. This article systematically analyzes key influences on product quality from five dimensions: raw materials, mold design, process parameters, production environment, and post-processing.
1. Raw Material Selection and Quality
Medical injection-molded products require materials with strict biocompatibility, chemical stability, and physical properties. For example, polypropylene (PP) is widely used in syringes due to its heat resistance and non-toxicity, while polycarbonate (PC) is preferred for high-precision devices owing to its transparency and impact resistance.
Key Factors:
-
Material Purity: Impurities or excessive additives may cause brittleness, discoloration, or harmful substance release.
-
Batch Consistency: Variations in flowability and shrinkage rates across batches can lead to dimensional deviations.
-
Certification Standards: Materials lacking FDA or ISO 10993 certification may pose biosafety risks.
Case: A company used unverified recycled plastic for infusion sets, resulting in excessive leachables and a product recall.
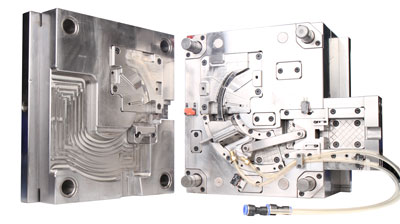
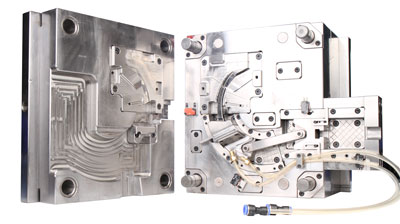
2. Mold Design and Manufacturing Precision
Molds are the "heart" of injection molding, with design rationality directly impacting dimensional accuracy, surface quality, and production efficiency.
Key Factors:
-
Runner System Design: Poor layout may cause uneven melt filling, leading to shrinkage or flash defects.
-
Cooling System Efficiency: Uneven cooling induces deformation or internal stress, reducing lifespan.
-
Mold Material and Surface Treatment: High-hardness steel (e.g., H13) with chrome plating reduces wear and extends mold life.
Case: A medical device firm faced a 30% drop in yield due to defective mold venting, causing surface gas marks.

3. Injection Molding Process Parameter Control
Parameters such as temperature, pressure, and speed must be precisely regulated. Deviations can trigger defects.
Key Factors:
-
Melt Temperature: Excessive heat degrades materials; insufficient heat causes filling deficiencies.
-
Injection Pressure and Speed: Low pressure leads to short shots; high speed may create weld lines.
-
Packing and Cooling Time: Inadequate packing causes shrinkage; insufficient cooling induces warping.
Case: A company set injection speed too high for cardiac stents, resulting in weld lines that failed biocompatibility tests.
4. Production Environment and Equipment Maintenance
Strict cleanliness and equipment stability are essential. Contamination or malfunctions pose systemic risks.
Key Factors:
-
Cleanroom Standards: Dust particles exceeding ISO 14644-1 limits may contaminate surfaces.
-
Equipment Precision and Maintenance: Worn screw barrels or faulty temperature control disrupt process stability.
-
Operator Compliance: Ungloved handling or uncleaned molds risk cross-contamination.
Case: A factory’s failed HVAC system raised humidity, causing product surface condensation and microbial test failures.
5. Post-Processing and Quality Inspection
Deburring, cleaning, and sterilization after molding also affect final quality.
Key Factors:
-
Deburring Methods: Residual burrs may injure tissues; automated laser deburring is preferred.
-
Cleaning and Drying: Inadequate cleaning leaves residues; ultrasonic cleaning + vacuum drying is ideal.
-
Sterilization Methods: Ethylene oxide (EO) residues require strict aeration; radiation may degrade materials.
Case: A firm’s insufficient aeration after EO sterilization led to toxic residue exceedances and regulatory penalties.
Conclusion
Quality control for medical injection-molded products is a systemic endeavor requiring strict oversight across raw materials, mold design, process parameters, production environments, and post-processing. As medical demands for safety and precision rise, firms must adopt digital management (e.g., MES systems), advanced inspection technologies (e.g., CT scanning), and continuous process optimization to build robust quality assurance frameworks. Only through such efforts can they earn trust and deliver reliable medical solutions to patients.










 Home
Home
