In the field of medical injection molding, product fracture is a core issue affecting production yield and clinical safety. From precision surgical instrument components to high-requirement implant shells, any micro-crack can lead to product rejection or even medical accidents. Combining the special needs of the medical industry, this article provides an in-depth analysis of the root causes of fractures in injection-molded products from four dimensions: materials, molds, processes, and equipment, and offers targeted solutions.
I. Material Selection and Handling: The "Invisible Killer" of Medical-grade Plastics
-
Uncontrolled Recycled Material Ratio
Medical products have extremely high requirements for material purity. A recycled material content exceeding 5% can lead to molecular chain breakage. In a case study of a cardiac stent housing, the brittleness rate increased by 300% due to the inclusion of 10% recycled material, resulting in product rejection. Solution: Strictly use new medical-grade raw materials certified by the FDA, such as polycarbonate (PC) and polyether ether ketone (PEEK), and establish a batch traceability system.
-
Moisture Management Failure
Hydroscopic materials like PPSU undergo hydrolysis when the humidity exceeds 0.2%. In one instance, an infusion set connector fractured during ejection due to inadequate drying (not subjected to 120°C/4-hour vacuum drying). Medical enterprises must implement a humidity monitoring system and adopt a "dual-temperature drying method" (80°C ordinary drying followed by 120°C vacuum drying) for materials like PA and PBT.
-
Additive Compatibility Issues
Incorrect lubricant addition caused material incompatibility in a dialyzer housing, leading to crazing during -40°C low-temperature testing. Medical injection molding must use USP Class VI-certified additives and verify material compatibility via Differential Scanning Calorimetry (DSC).
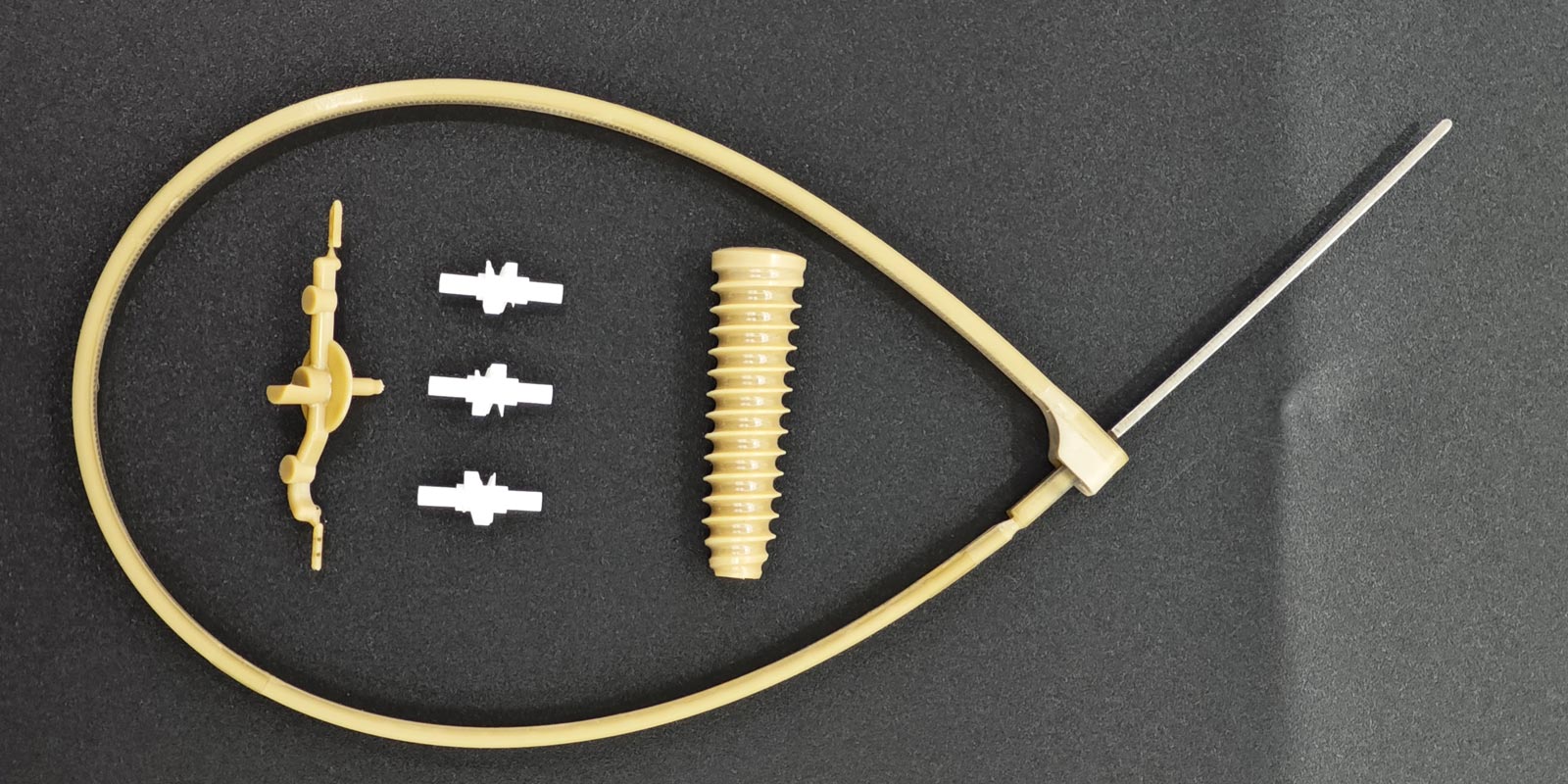
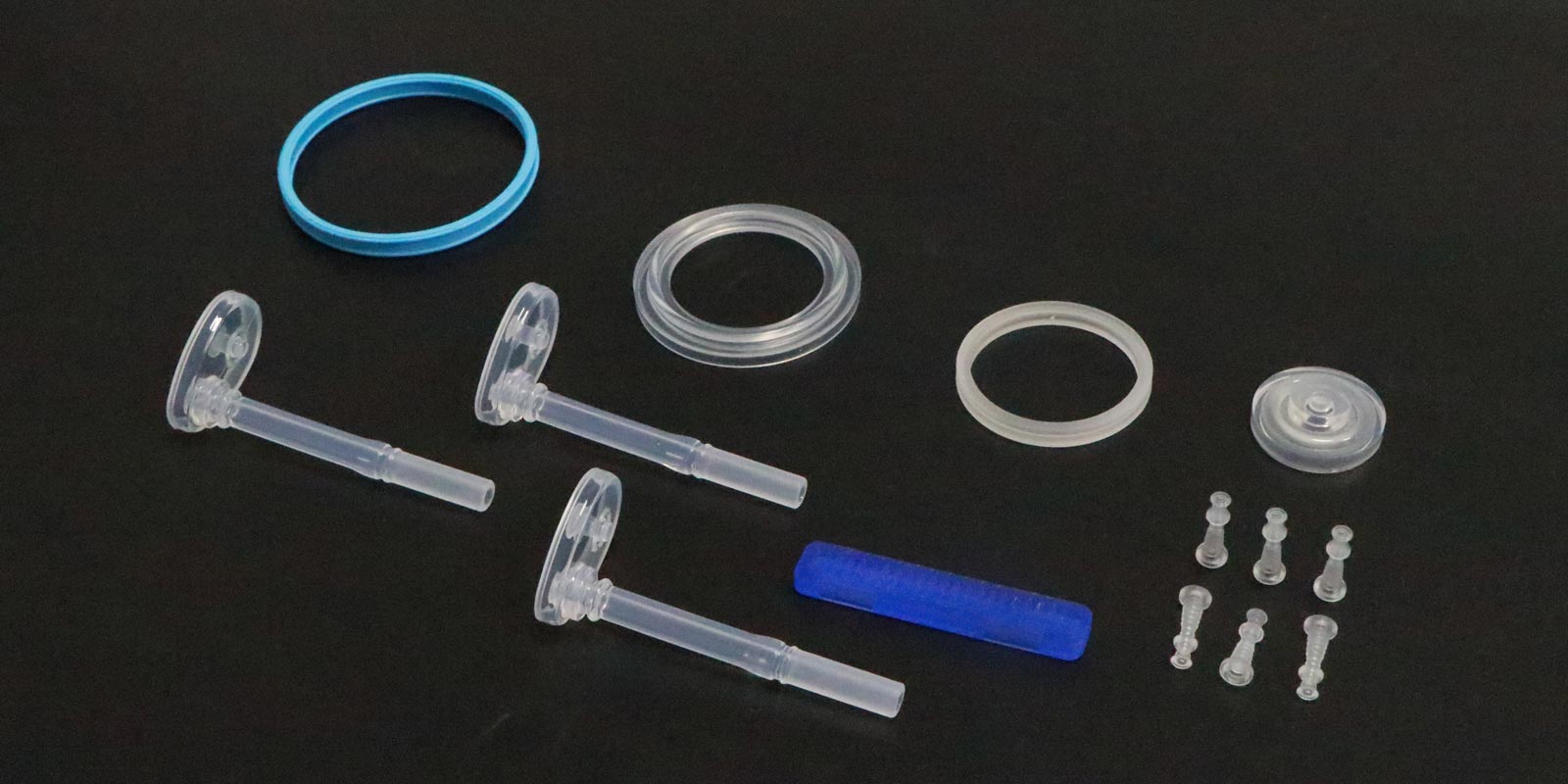
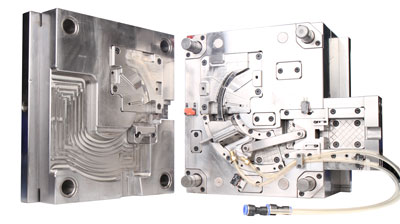
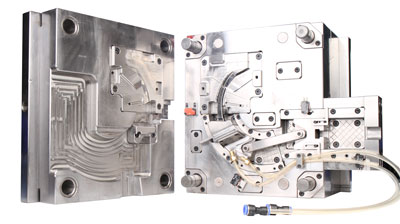
II. Mold Design: The "Genetic Defect" of Medical Precision
-
Ejection System Imbalance
An insulin pen component fractured at a 0.3 mm thin-wall section due to improper ejector pin layout. Medical molds require a "multi-point progressive ejection" design, with ejector pin diameters ≤0.5 mm assisted by nitrogen gas springs and an increased draft angle of 0.5° compared to ordinary products.
-
Runner System Defects
A minimally invasive surgical forceps handle developed residual stresses of 85 MPa (far exceeding the 30 MPa limit for medical products) due to a direct gate design. Switching to a hot runner + needle valve gate reduced stress to 18 MPa. Medical molds should prioritize hot runner systems with gate diameters controlled at 60%-80% of the product wall thickness.
-
Insert Structure Risks
A 200 μm micro-crack formed at the interface of an orthopedic implant due to a 0.8% shrinkage rate mismatch between the metal insert and PEEK. Solution: Preheat inserts (temperature controlled at Tg ±10°C) and design a 0.1 mm transition layer.

III. Process Control: The "Lifeline" of Medical Quality
-
Injection Parameter Out of Control
A blood collection tube fractured due to excessive injection speed (300 mm/s), causing molecular chain orientation stress. Medical injection molding requires a "three-stage injection" protocol:
-
First stage (70% filling): Speed ≤100 mm/s
-
Second stage (packing): Pressure gradient control (5% pressure reduction per 5% filling)
-
Third stage (cooling): Mold temperature fluctuation ≤±1°C
-
Crystallization Control Failure
PEEK materials are prone to abnormal crystallization above 380°C. An artificial joint component showed a 40% reduction in mechanical properties due to a 15% crystallinity deviation. An infrared crystallinity online detection system should maintain crystallinity within 55%-65%.
-
Post-processing Defects
A dialysis membrane stent fractured due to improper annealing (temperature fluctuation ±5°C), causing uneven residual stress release. Medical products require a "stepped annealing" process:
-
60°C/2h (eliminate orientation stress)
-
100°C/1h (eliminate cooling stress)
-
140°C/0.5h (eliminate conformational stress)
IV. Equipment Maintenance: The "Invisible Shield" of Medical Safety
-
Screw Wear Exceeding Limits
An infusion pump housing developed a 150 μm gap at the weld line due to screw wear causing poor plasticization. Medical injection molding machines require monthly laser interferometer inspections, with screw-barrel clearance maintained at 0.05-0.1 mm.
-
Hydraulic System Contamination
A 20% fluctuation in mold opening/closing impact force (due to hydraulic oil contamination) caused hidden cracks in an endoscope component. Medical enterprises must install a dedicated hydraulic system with triple filtration (5 μm → 1 μm → 0.1 μm precision).
-
Temperature Control System Failure
A 3°C sensor deviation in the barrel temperature caused material degradation in an anesthesia mask. Medical injection molding machines require dual-sensor redundancy and a "three-mode calibration" (no-load/full-load/production state calibrations).
V. Special Requirements in the Medical Industry
-
Biocompatibility Verification
All fractured products must undergo ISO 10993 biocompatibility testing, focusing on:
-
Cytotoxicity (L929 cell viability ≥80%)
-
Sensitization (GPMT test negative)
-
Genotoxicity (Ames test negative)
-
Cleanliness Control
Fracture surfaces must meet ISO 14644-1 Class 5 cleanliness, with ≤10 particles ≥5 μm per cm² detected by laser particle counters.
-
Traceability System Construction
Establish a "five-dimensional traceability system":
-
Raw material batch
-
Mold usage cycles
-
Process parameter sets
-
Equipment maintenance records
-
Operator information
The prevention of fractures in medical injection-molded products essentially requires the implementation of a medical Quality Management System (QMS). From DFMEA to PFMEA, and from SPC to APQP, every link must embody a "zero-defect" philosophy. When a cardiac pacemaker housing manufacturer reduced the fracture rate from 0.3% to 0.002%, its core experience was quantifying every parameter into measurable quality indicators, constructing a complete protective chain from molecular chains to clinical applications.










 Home
Home
