In the field of medical injection molding, product surface cleanliness is paramount to ensuring the safety, functionality, and durability of medical devices. However, surface contamination issues—such as residual stains, oil spots, dust, or color defects—remain prevalent in actual production. These problems not only reduce product qualification rates but also pose risks of medical malpractice. This article delves into the root causes of surface contamination from four key perspectives: materials, processes, molds, and environmental control, while offering systematic solutions to address these challenges.
1. Material Factors: The Hidden Sources of pollution
1.1 Impurities in Raw Materials
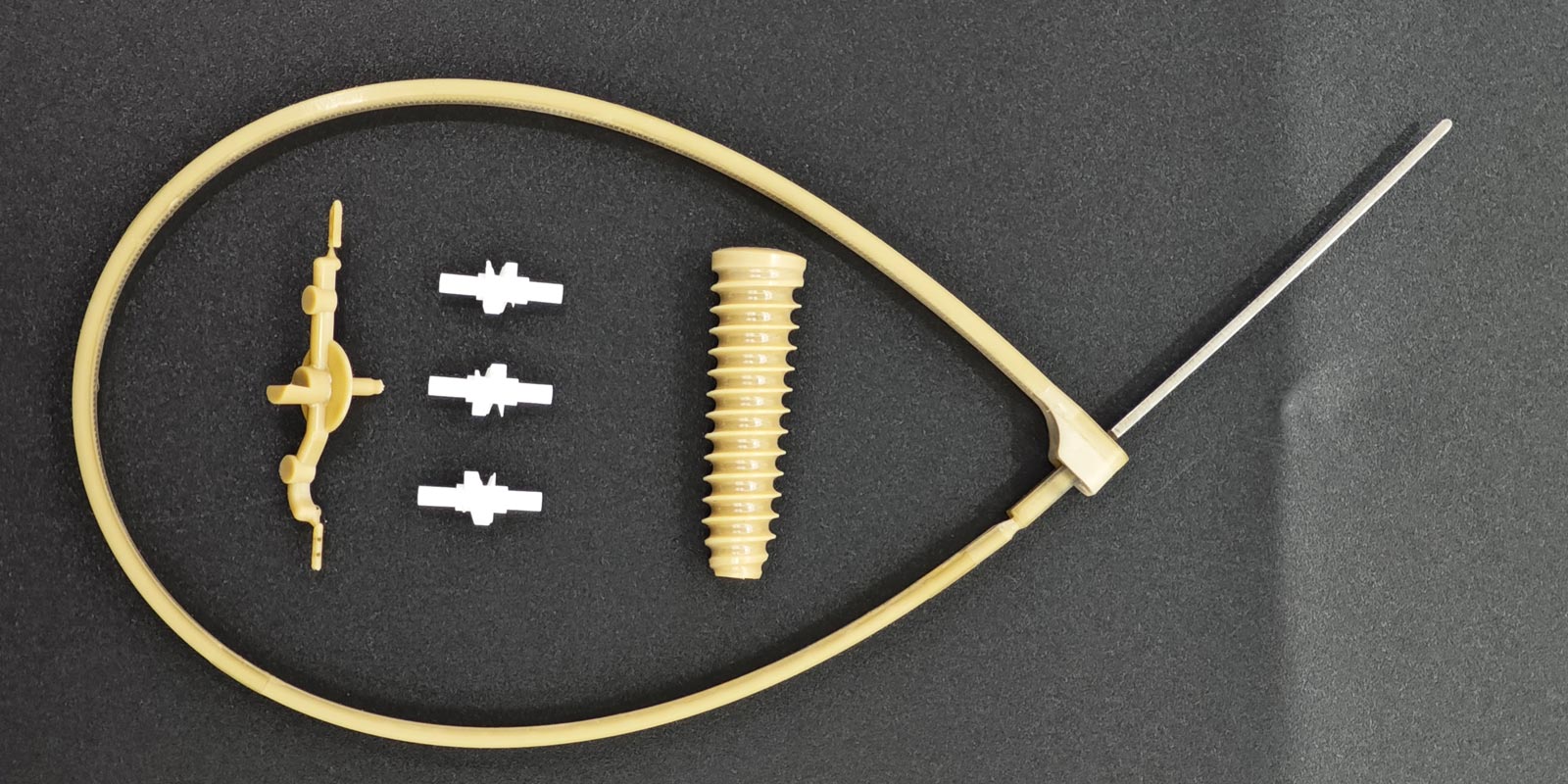
Medical-grade plastics (e.g., PC, PP, PPSU) containing impurities or low-molecular-weight volatiles can decompose under high temperatures, leaving residues on mold surfaces. For instance, inadequately dried materials may cause surface water streaking due to moisture vaporization.
1.2 Additive Migration
Lubricants or antistatic agents added to enhance performance may exude onto surfaces if incompatible with the base material. A recall incident involved an infusion set with excessive lubricant, leading to bacterial adhesion.
1.3 Uneven Dispersion of Color Masterbatch
Insufficient mixing of color masterbatch and base resin results in localized color defects. Medical products demand strict color consistency, as deviations affect device identification.
Solutions:
-
Use ISO 10993-certified raw materials and establish a supplier whitelist.
-
Pre-dry materials with dehumidifying dryers to control moisture content ≤0.02%.
-
Optimize masterbatch ratios and enhance mixing via twin-screw extruders.

2. Process Parameters: The Imbalanced "Temperature-Pressure-Time" Triangle
2.1 Abnormal Melt Temperature
Excessive heat degrades materials (e.g., PVC decomposes above 180°C), producing carbonized particles. Insufficient heat causes filling defects, leaving flow marks. A catheter connector manufacturer faced periodic surface stains due to ±5°C barrel temperature fluctuations.
2.2 Insufficient Injection Pressure
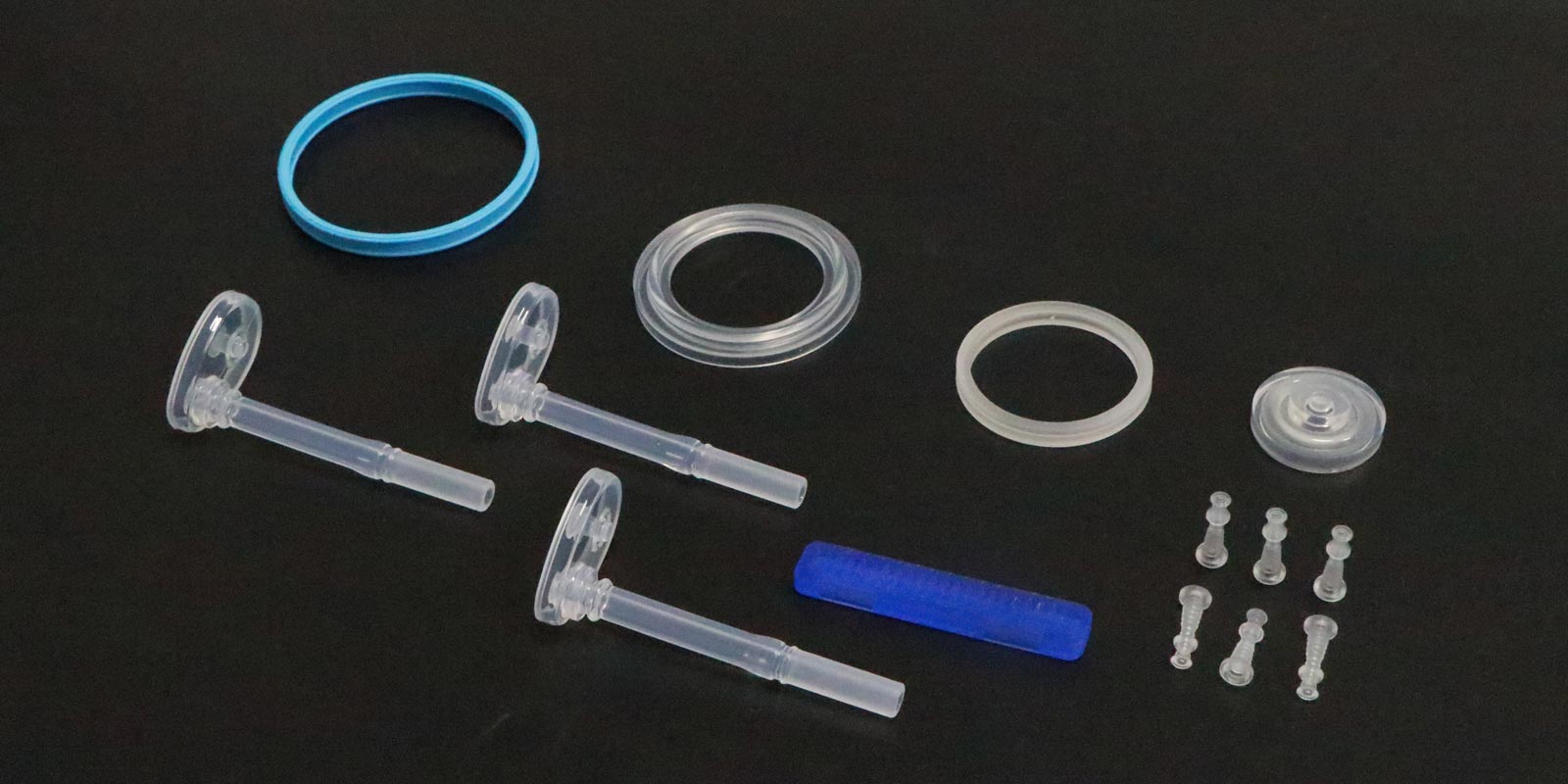
Low pressure prevents complete mold filling, creating burrs or sink marks that trap contaminants. Medical microfluidic chips require flow channel precision of ±0.001mm, demanding pressure control at 0.1 MPa increments.
2.3 Short Holding Time
Inadequate holding pressure leads to internal stress, causing surface cracks that harbor microorganisms.
Solutions:
-
Monitor melt temperature with infrared sensors and maintain ±1°C stability via PID control.
-
Adopt multi-stage injection: high-speed filling followed by low-pressure compensation.
-
Optimize holding curves using Moldflow simulation to ensure uniform density (≥99%).
3. Mold Defects: Microscopic "Pollution Traps"
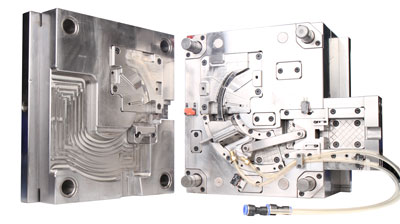
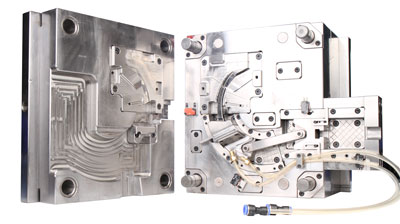
3.1 Poor Exhaust System Design
Molds lacking exhaust slots trap gases, creating burn marks. Medical-grade LCP requires exhaust slots depth of 0.01–0.03mm due to its low viscosity.
3.2 Excessive Cavity Surface Roughness
A roughness (Ra) >0.8μm increases mold release agent adhesion, leaving mirror-like stains. An artificial joint component with Ra1.6μm caused postoperative infections.
3.3 Cooling Water Contamination
Scale buildup in cooling channels distorts products via localized overheating. Medical molds demand deionized water cooling with regular EDI treatment.
Solutions:
-
Laser-etch exhaust slots to avoid microcracks from traditional EDM processing.
-
Apply nano-coatings (e.g., diamond-like carbon) to reduce surface energy.
-
Integrate temperature sensors and flow meters for real-time cooling system monitoring.
4. Environmental Control: The Overlooked "Clean Barrier"
4.1 Inadequate Cleanroom Standards
Medical injection molding requires ISO Class 7 (10,000-grade) cleanrooms, but some facilities use ordinary rooms, resulting in 300x higher airborne particles (≥0.5μm), directly contaminating products.
4.2 Human-Induced Pollution
Operators without cleanroom garments shed ~100,000 skin flakes per minute. Gloves replaced less frequently than every 2 hours significantly increase contamination risks.
4.3 Packaging Material Off-Gassing
Low-quality PE bags release plasticizers, as seen in a blood glucose meter case where packaging caused oily residue on detection windows.
Solutions:
-
Deploy FFU units to maintain ≥10 Pa pressure differentials and ≥25 air changes/hour.
-
Use AI vision systems to monitor attire compliance (99.7% accuracy).
-
Select USP Class VI-certified packaging with supplier audits.
5. Quality Management System: From Reactive Repair to Proactive Prevention
5.1 Implement APQP (Advanced Product Quality Planning)
Identify critical-to-cleanliness (CTC) characteristics during product development. One firm reduced 12 contamination risks via DFMEA analysis.
5.2 Establish SPC Control Charts
Monitor key parameters (e.g., melt temperature, pressure) using X-bar charts to achieve Cpk ≥1.67.
5.3 Promote 5S+1S (Safety) Management
Organized workspaces reduced equipment dust accumulation by 82% in one case.
Conclusion
Achieving surface cleanliness in medical injection molding requires a multidisciplinary approach integrating material science, fluid mechanics, and microbiology. Enterprises must establish end-to-end traceability systems and leverage IoT for real-time data analytics. Only by embedding quality awareness into every process detail can they thrive under stringent medical regulations.










 Home
Home
